Medicine is the science and practice of diagnosing, treating, and preventing diseases and injuries. Throughout history, sustained medical advancements have saved or improved the lives of millions of people worldwide. In fact, since the discovery of antibiotics alone, the average global life expectancy has increased by over 20 years.
A specific example is the story of James Phipps, the first person ever to be vaccinated. In 1796, at just 8, Phipps was inoculated with cowpox by Edward Jenner to test his hypothesis that it would protect him from smallpox. This brave and pioneering experiment laid the foundation for what we now know as vaccines. But these leaps in health wisdom have resulted from centuries of scientific discoveries, trial and error, and innovation. Some of those light-bulb moments were accidental, others intentional, and a few even controversial.
To satisfy your curiosity, let’s delve into the birth of eight historical medical creations, their discovery, and why those inventions matter to us.
Content:
- The Thermometer: Measuring Body Temperature
- The Stethoscope: Listening to the Heart and Lungs
- The X-Ray: Peeking Inside the Body
- Antibiotics: Fighting Bacterial Infections
- The Electrocardiograph: Documenting the Heart’s Electrical Activity
- Insulin: Treating Diabetes
- The Artificial Heart: Replacing the Failing Engine
- Magnetic Resonance Imaging: Mapping the Brain’s Function
Today’s Focus of Attention is reader-supported. We sometimes include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission.
The Thermometer: Measuring Body Temperature
This device measures and displays the body’s thermal state in a person or animal and is useful in detecting fever and infections, common signs of many diseases.
History
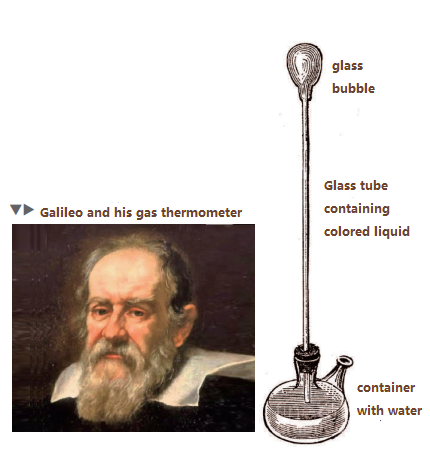
Circa 1592, Galileo Galilei built the thermoscope, the first instrument showing the variation of temperature. It used water and air to show the changes in hotness or coldness but didn’t have a scale to measure the exact heat.
In 1612, an Italian physician, Santorio Santorio, added a numerical range to the thermoscope he had to capture the body temperature of his patients. However, his device was bulky, impractical, and slow.
Around 1654, Ferdinand II, the Grand Duke of Tuscany, created the first enclosed liquid-in-a-glass thermometer, which used alcohol as the fluid with a scale of 50 degrees.

Fahrenheit’s Legacy
A few decades later, in 1709, Daniel Gabriel Fahrenheit, a Polish-born Dutch physicist, developed a more exact and reliable alcohol thermometer.
And just five years afterwards, he came up with the faster mercury thermometer. After this, he introduced the Fahrenheit scale, which divided the freezing and evaporation points of water by 180 degrees.
Celsius’ Contribution
After a couple of decades, the Swedish astronomer Anders Celsius created the Celsius scale. Back then, it was the opposite of the modern system, with 0 as the boiling point of water and 100 as the ice point. Carolus Linnaeus, a Swedish botanist, reversed it in 1744.
The Celsius scale, also known as centigrade, is used in most countries and scientific fields.
Compact and Quick
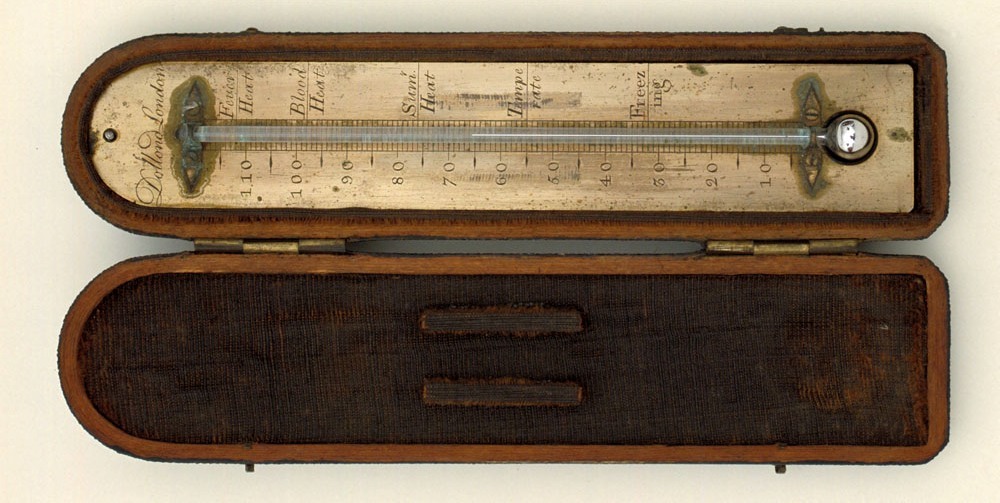
A little more than a century later, in 1867, Thomas Allbutt, an English physician, invented the first portable medical thermometer that recorded the temperature in five minutes.
Before that, thermal detectors were a foot long and took 20 minutes to measure body heat.
Into the 20th Century
At the dawn of the 1900s, several new types of thermometers were developed, including the ear, infrared, and digital. All of them use different methods and technologies to read the temperature, such as the tympanic membrane, temporal artery, or electronic heat sensors.
“In all of science, there is nothing so beneficial to man as the art of medicine.”
Hippocrates
The Stethoscope: Listening to the Heart and Lungs

The stethoscope allows doctors and other health professionals to listen to the sounds of organs inside the body, helping in the diagnosis of heart murmurs, arrhythmias, asthma, bronchitis, pneumonia, and more.
René Laennec, a French physician, invented the device on a wooden tube to amplify the sounds of the heart and lungs.
Origins of The Stethoscope
In 1816, Laennec was examining a young woman with a cardiac issue. He wanted to listen to her heartbeat, but he felt uncomfortable placing his ear on her chest, a common practice in old times. He also knew that her clothes and breasts would muffle the sound.
Then he remembered that he’d seen children transmit sound by scratching a pin at one end of a long piece of wood while listening to the other end. So, he gave it a try.
He rolled up a sheet of paper into a cylinder and placed one end on her chest and the other in his ear. He was amazed to hear her heart sounds much more clearly than ever before. He called his invention ‘stethoscope’, from the Greek words for ‘chest’ and ‘examine.’ Laennec improved his design by hollowing out a piece of wood and experimenting with different shapes and sizes of the chest and ear pieces.
After perfecting his idea, he was able to listen to the sounds of the lungs, abdomen, and blood vessels and discovered many new signs and symptoms of chest diseases. Furthermore, he could tell the difference between normal and abnormal breathing, fluid in the lungs, and the variations of heart beats in different conditions.


In 1819, he published his findings and his description of the stethoscope in a book titled “De l’Auscultation Mediate” (On Mediate Auscultation).
Just a few years later, Laennec’s stethoscope became the standard for chest examinations.
Reinventing Ausculation

In the course of time, other inventors modified and improved the stethoscope. Charles Williams added a flexible tube; Arthur Leared and George Cammann made it binaural; and David Littmann enhanced its acoustic quality.
“I saw and heard, as it were, the noise of the heart valves in action; a phenomenon which I do not believe has ever been observed before me.”
René Laennec
The X-Ray: Peeking Inside the Body
The X-ray is electromagnetic radiation that penetrates various materials and produces images of the internal structures of the body. This powerful tool is functional for medical diagnosis and treatment, as well as for scientific and industrial applications.
Beginnings
Wilhelm Rontgen discovered the X-rays in 1895 while he was experimenting with a cathode ray tube, a glass tube with electrodes at both ends, and a vacuum inside.
When the high voltage ran through the electrodes, a beam of electrons formed within the tube. Then, Rontgen noticed that a nearby screen coated with barium platinocyanide, a fluorescent material, glowed while the tube was operating, even when it was covered with thick cardboard.

He realised invisible rays were coming out of the tube and reaching the screen, calling them “X-rays” because of their unknown origin. Rontgen started investigating the properties of the mysterious rays and found that they passed through paper, wood, and metal, but not through bones or lead. He also spotted the shadows of solid objects on photographic plates, so he decided to test the X-rays with his own hands and placed them between the tube and a plate.
The First Radiography
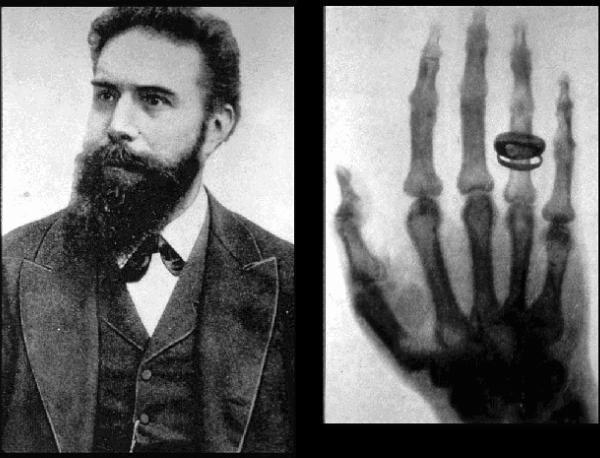
The image of his bones and his wedding ring on the plate became the earliest X-ray photograph of a human body part ever.
In a paper titled “On a New Kind of Rays,” Rontgen published his revelation and sent copies of his study and radiographies to several prominent scientists and physicians. It caused a sensation and made front-page news.
Wilhelm Rontgen received many honours and awards for his discovery, including the first Nobel Prize in Physics in 1901. He donated the award money to his university and continued his research until his death in 1923.
“I did not think; I investigated.”
Wilhelm Rontgen
Antibiotics: Fighting Bacterial Infections
Antibiotics are substances that kill or inhibit the growth of bacteria, which cause infections and diseases in humans and animals. Since their discovery in the 20th century, they have saved millions of lives and revolutionised the field of medicine.
Genesis
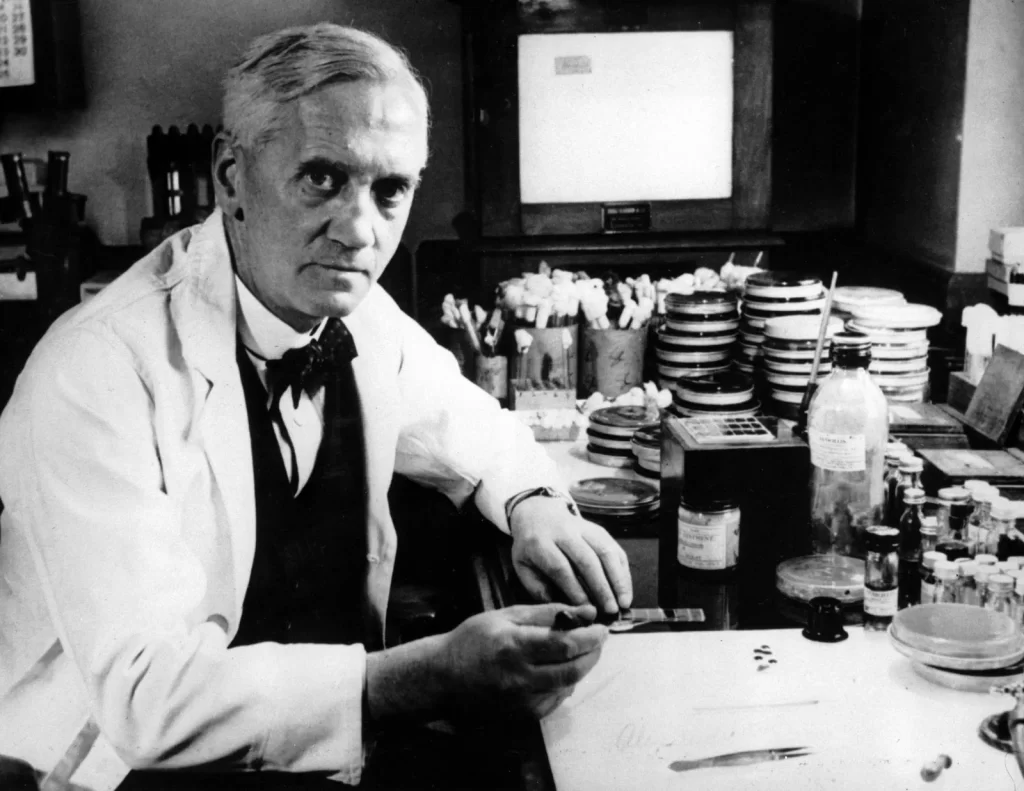
Alexander Fleming, who studied medicine in London and became a bacteriologist, was interested in the natural antibacterial substances produced by the human body and some microorganisms.
His interest surfaced when he served as a captain in the Royal Army Medical Corps during World War I and witnessed countless soldiers die from infected wounds.
In 1928, Fleming was working on the culture of Staphylococcus bacteria, a common cause of skin infections, boils, and pneumonia.
Accidental Discovery
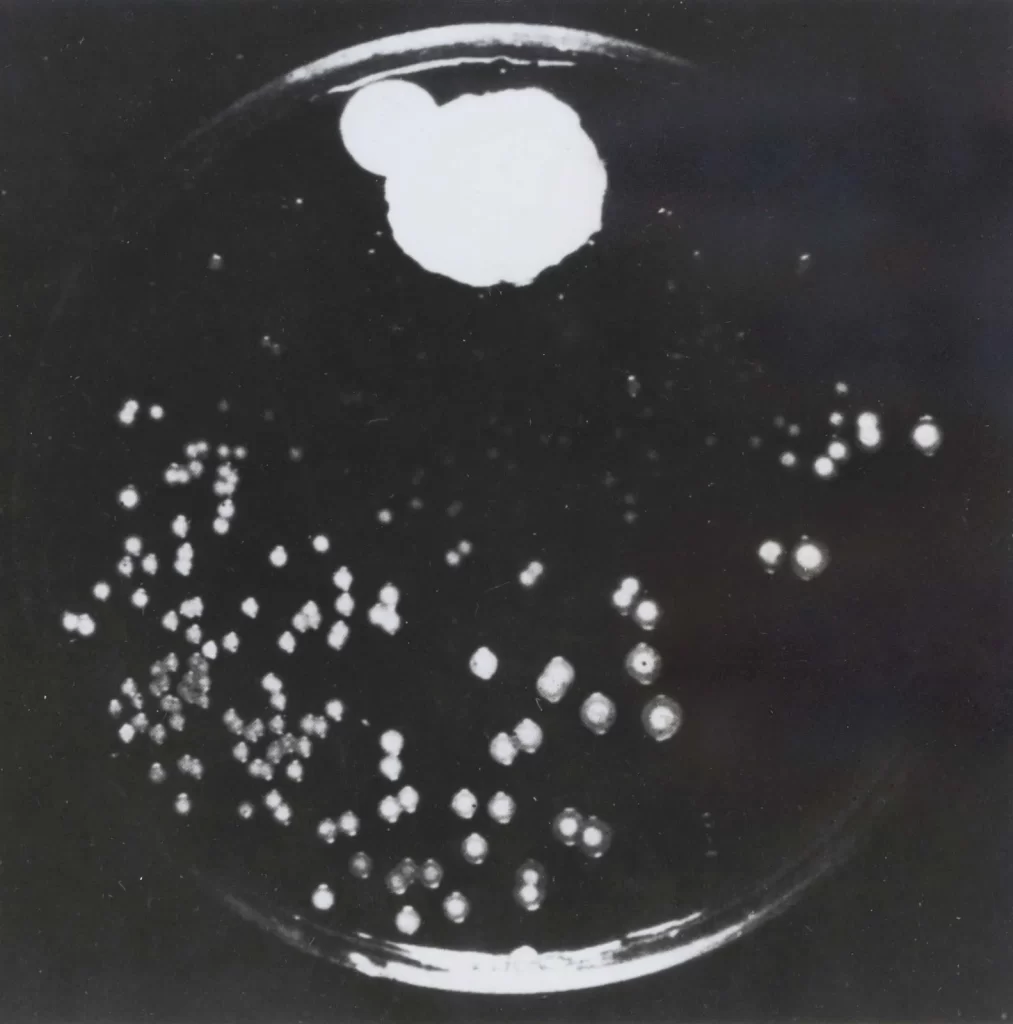
Before going on holiday, Fleming had left a few culture plates in his laboratory. But when he returned, he noticed that one plate had been contaminated by a mould called ‘Penicillium notatum.’
He likewise detected that the bacteria around the mould had been killed or prevented from growing, creating a clear zone. At that moment, Fleming realised that the mould had produced a substance with an antibacterial effect and named it ‘penicillin’ after the name of the mould.
In 1929, Fleming published his discovery in the British Journal of Experimental Pathology, but with no resources or expertise, he couldn’t isolate and purify penicillin. Moreover, the scientific community showed scepticism and indifference because they considered penicillin too unstable and weak to be used as a drug.
Determined, Fleming continued his research but did not pursue its development as a medicine.
From Obscurity to Medical Marvel
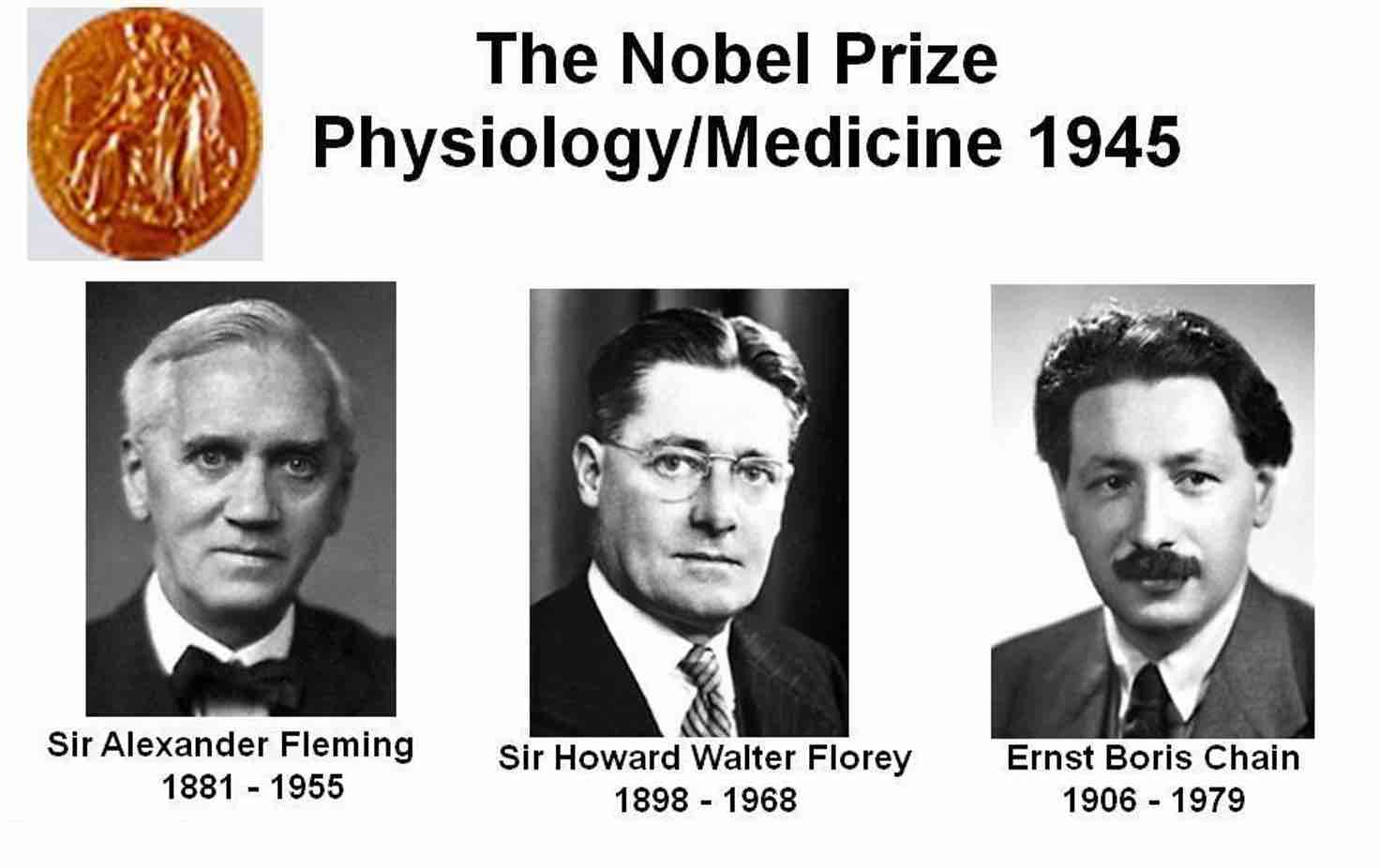
It wasn’t until 1939 that a team of experts from the University of Oxford, led by Howard Florey and Ernst Chain, reviewed Fleming’s work on penicillin.
They extracted and purified penicillin and tested its efficacy and safety on mice and humans, finding that penicillin was a powerful and nontoxic antibiotic for various bacterial infections, including septicaemia, meningitis, and pneumonia.
Both scientists collaborated with British and American pharmaceuticals to mass-produce penicillin during World War II to treat wounded soldiers and civilians.
In 1945, Fleming, Florey, and Chain shared the Nobel Prize in Physiology for their discovery and success. The identification of penicillin opened the door for the development and synthesis of many other antibiotics, such as streptomycin, tetracycline, and erythromycin.
“One sometimes finds what one is not looking for.”
Alexander Fleming
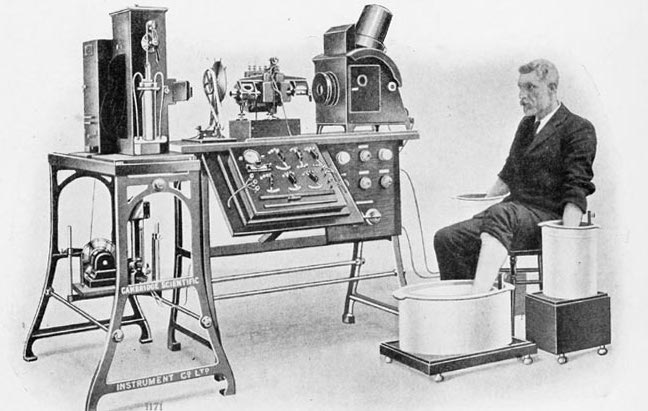
The Electrocardiograph: Documenting the Heart’s Electrical Activity
This tool, invented by Willem Einthoven, records the electric impulses of the heart and produces a graph called an electrocardiogram, or ECG. It’s useful for diagnosing and monitoring arrhythmias, cardiac arrests, and heart failure.

History of The Electrocardiograph
In 1893, Einthoven attended a lecture by Augustus Waller, a British physiologist, who showed the first human electrocardiogram using a capillary electrometer, a device that detected electric currents from the movement of a liquid in a tube. While impressed by Waller’s work, Einthoven realised that the capillary electrometer was too slow and insensitive to record the subtle changes in the heart’s electrical activity. Thus, he decided to develop a better instrument for that purpose.
The Birth of ECG
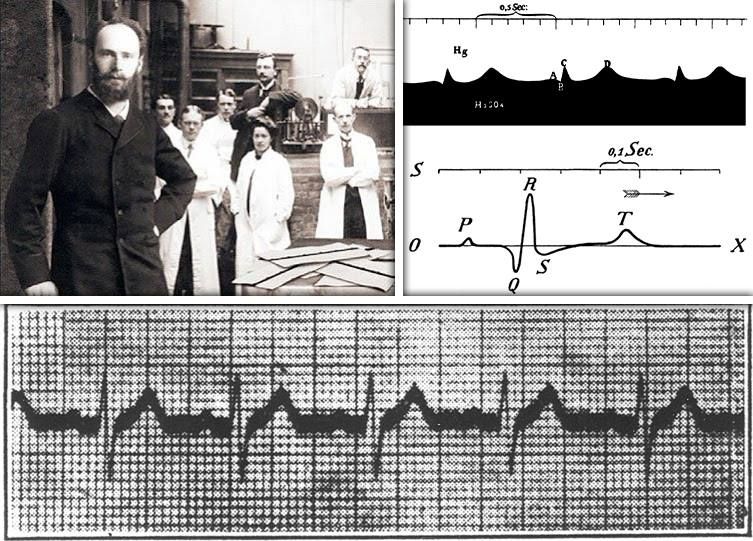
A few years later, in 1901, Einthoven invented the string galvanometer, a device consisting of a thin silver-plated quartz wire stretched between two electromagnets.
When an electric current passed, the wire vibrated and deflected a beam of light onto a moving piece of photographic paper. This device, much more sensitive and accurate than Waller’s invention, recorded the heart’s bioelectrical signals in greater detail and speed.
Einthoven called his graph an electrocardiogram and assigned the letters P, Q, R, S, and T to the different waves and segments of the chart.
Pioneering Diagnostics
In 1902, he made the first record of a human heart using his invention. He connected electrodes to the arms and legs of a patient and transmitted the signals to his device in his laboratory, one and a half kilometres away from the medical centre.
Connecting via telephone with the hospital staff, Einthoven was able to register the normal and abnormal patterns of the heart’s bioelectricity and correlate them with the clinical symptoms and signs of the patient.
He also established the standard 12-lead system for recording the ECG from different angles and perspectives.
Four years afterwards, Einthoven published his paper on the ECG and its applications, describing the normal and abnormal ECGs of cardiac conditions such as atrial fibrillation, ventricular tachycardia, heart block, myocardial infarction, and pericarditis. Einthoven received the Nobel Prize in Physiology in 1924, donated the money to the University of Leiden, and continued working until he passed away in 1927.
“It is not enough to have a good mind; the main thing is to use it well.”
René Descartes
Insulin: Treating Diabetes
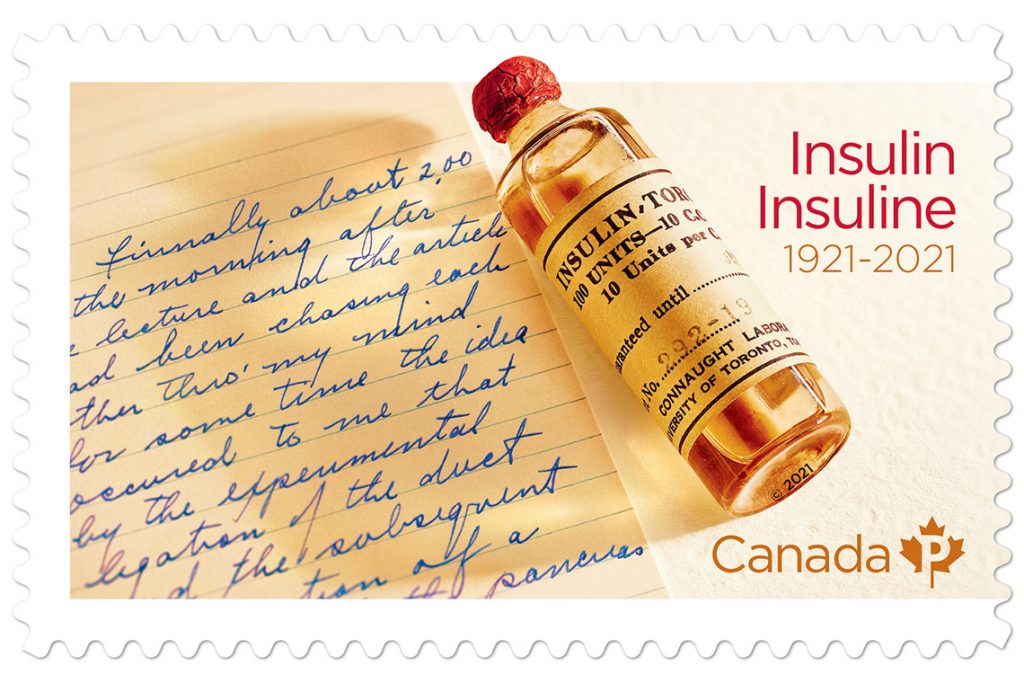
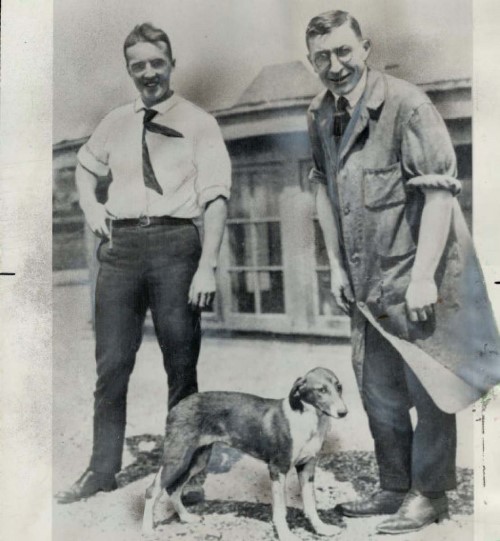
Discovered by Frederick Banting and Charles Best, insulin is a hormone that aids the body in controlling the quantity of glucose in the blood. People with diabetes have either a lack of or a resistance to insulin’s action, causing high blood sugar levels and other health problems.
Background
While serving as a surgeon in World War I, Canadian Frederick Banting became interested in diabetes and the role of the pancreas in regulating glucose levels. He considered extracting the pancreatic secretions that lowered blood sugar from healthy dogs and injecting them into diabetic dogs.
In the summer of 1921, Banting received a small grant and a lab space to conduct his experiments on diabetes. In need of help, the lab assigned American biochemist Charles Best as Banting’s assistant. B&B started their research by removing the pancreas from healthy canines, making them diabetic.

Then, they tied off the pancreatic ducts of another group of dogs, stopping the flow of digestive juices and causing the pancreas to degenerate, leaving only the islets of Langerhans, the clusters of cells that produce insulin.
Both scientists extracted the islet tissue from these dogs and made a crude solution, calling it “isletin.” Following this, they injected the solution into the diabetic canines and found that it lowered their blood sugar levels and improved their symptoms.
A Leap Forward
Banting and Best understood they’d discovered a potential treatment for diabetes, but they needed to purify and test their extract further. So, they worked with the biochemist James Collip, who refined and made the substance more potent and less toxic.
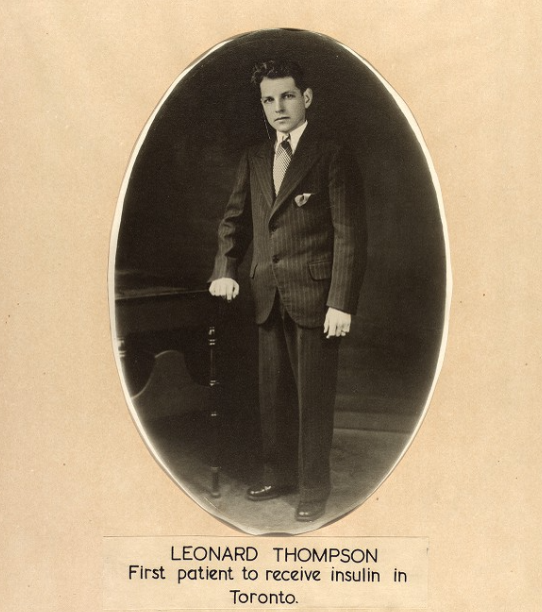
In 1922, B&B treated the first human patient with diabetes, a 14-year-old boy named Leonard Thompson, who was dying from the disease at the Toronto General Hospital. They injected him with their insulin extract, and his blood sugar levels dropped overnight.
The boy recovered from his diabetic coma and lived for another 13 years with regular insulin injections.
The discovery of the effect of insulin on the body awarded Banting and Best the Nobel Prize in Physiology in 1923, as the society hailed their study as a medical miracle and a novel treatment for diabetes.
“Insulin is not a cure for diabetes; it is a treatment. It enables the diabetic to burn sufficient carbohydrates so that proteins and fats may be added to the diet in sufficient quantities to provide energy for the economic burdens of life.”
Sir Frederick Banting
The Artificial Heart: Replacing the Failing Engine
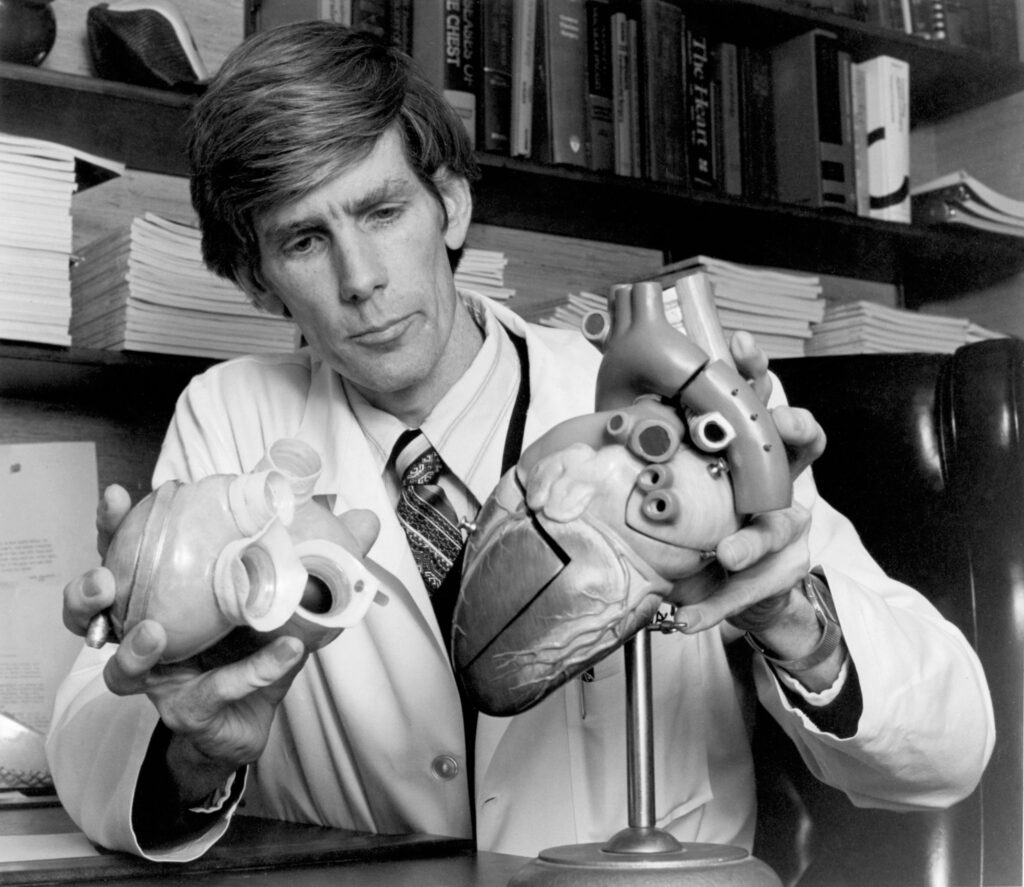
An artificial heart replaces the function of a natural heart, serving as a lifesaving option for people with end-stage failure and are waiting for a transplant. The mastermind behind this invention was the American physician and engineer Robert Jarvik.
Biography
Born in 1946 in Michigan, US, Jarvik studied medicine and engineering, later shifting his interests to the sphere of engineered organs.
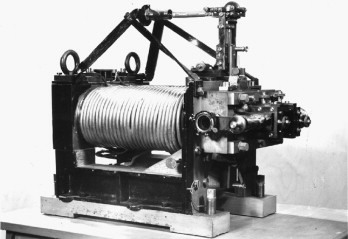
During his work as a researcher at the University of Utah, Jarvik joined the artificial heart programme led by the pioneer in the field, Willem Kolff. Jarvik designed and developed the Jarvik-7, the first plastic and metal lab-created coronary structure intended to last a lifetime.
With a capacity to pump up to 9.5 litres of blood per minute, J7 comprised two ventricles, four mechanical valves, and was connected to an external console for power and control.


A Medical Milestone
In 1982, Jarvik and his team implanted the J7 in the first human patient, Barney Clark, a 61-year-old dentist suffering from severe coronary failure. William De Vries, a cardiothoracic surgeon, performed the surgery at the University of Utah Medical Centre.
The patient survived 112 days with the Jarvik-7, becoming the earliest person to live with a permanently manufactured central circulatory organ.
The artificial heart offers hope and improves the quality of life for many people with cardiovascular issues or those who are still waiting for a transplant.
Jarvik’s Legacy
Jarvik spent the decades after his headline-making breakthrough refining smaller ventricular assist devices such as the Jarvik 2000 and the paediatric Jarvik 2015, work that earned him a lifetime-achievement award in 2018.
Sadly, he died on 30 May 2025 in Manhattan, aged 79, from complications of Parkinson’s disease, his wife—writer Marilyn vos Savant—announced. Colleagues like Houston heart-surgery innovator Dr O. H. Frazier hailed him as “a giant who gave heart-failure patients precious time.”
Jarvik’s pioneering device has evolved into successors such as the SynCardia Total Artificial Heart, implanted in more than 1,700 patients worldwide.
“The artificial heart is not a pump; it’s an environment.”
Robert Jarvik
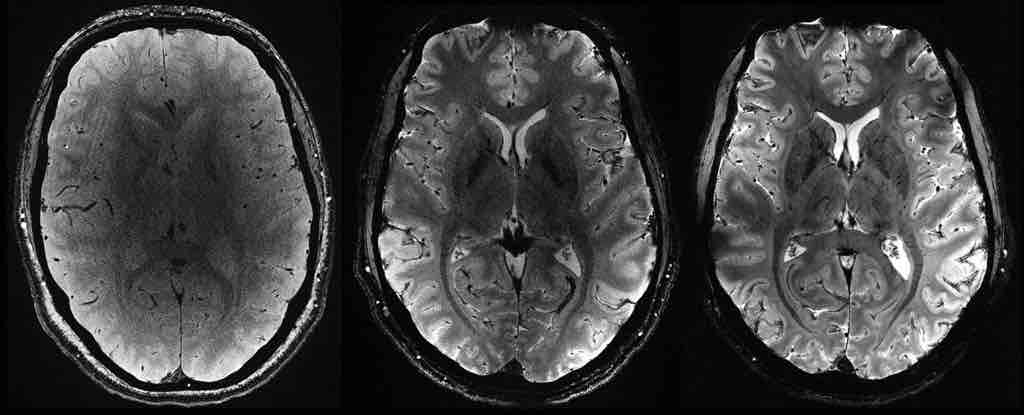
Magnetic Resonance Imaging: Mapping the Brain’s Function
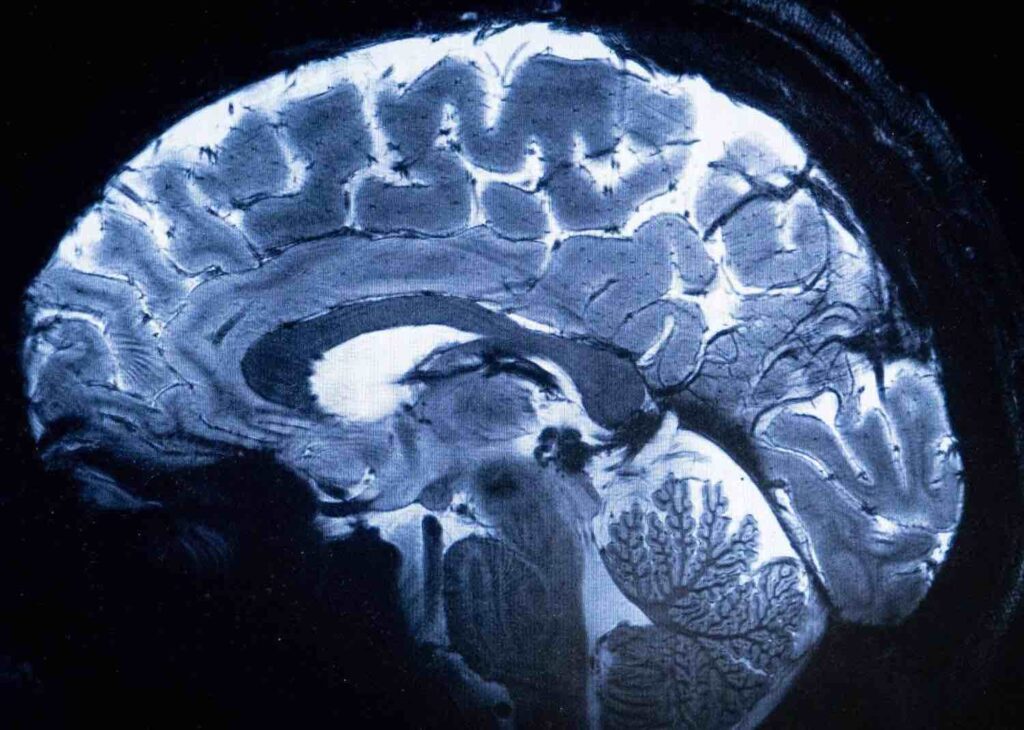
This technique uses magnetic fields to measure the changes in brain activity based on the blood oxygen level. It was developed by the Japanese physicist Seiji Ogawa, who used the blood oxygen level dependent (BOLD) contrast to detect variations in blood flow and oxygenation in the cerebral matter.


With studies in physics and engineering, Seiji Ogawa worked as a researcher at the Toshiba Research and Development Centre and the AT&T Bell Laboratories.
In 1990, Ogawa found that when a brain sector is activated by a stimulus or a task, the blood stream, and oxygen consumption in that region increased, causing a change in the ratio of oxygenated haemoglobin (HbO) and deoxygenated haemoglobin (dHb).
Since dHb is more magnetic than HbO, it affects the resonance signal more strongly. So, Ogawa realised that by measuring the changes in the signal, he could map the mental processing related to the blood oxygen levels. This is the basis of an MRI.
He published his findings in 1990 and 1992 and showed the first magnetic resonance images of the human brain.
Unravelling the Mind
Ogawa’s invention of the BOLD contrast and MRI was a breakthrough in neuroscience and neuroimaging, enabling clinicians and researchers to study the brain’s function and structure in a non-invasive, safe, and high-resolution way.
Apart from that, it allowed them to investigate the neural correlates of emotional and behavioural processes, such as perception, memory, language, emotion, and decision-making.
Magnetic Resonance Imaging has also been used to diagnose and monitor neurological and psychiatric disorders, including Alzheimer’s, Parkinson’s, schizophrenia, depression, and autism.
By comparing the patterns of healthy and diseased brains, MRI can help identify the regions and networks affected by these diseases.
“The true method of knowledge is experiment.”
William Blake
It’s crucial to understand the enduring legacy of these groundbreaking innovations and how they continue to influence present-day medicine. To illustrate, the discovery of X-rays set the stage for modern radiology, which now includes MRIs, CT and PET scans, providing detailed images of the body’s internal structures and aiding in early and accurate diagnoses. But it doesn’t stop there. Nowadays we have gene editing, for instance, and other medical breakthroughs that involve the use of AI. The possibilities are limitless.


